A coronary artery calcium ( CAC ) scan, which detects and measures calcium deposits in the arteries, is being hailed as a life-saving test for heart disease prevention. The non-invasive test scores from zero up into the thousands, with higher scores indicating greater risk of heart attack. TOI spoke to Dr Shailesh Singh, consultant cardiologist at Fortis Escorts , Delhi, about when CAC helps — and when it misleads
“CAC has revolutionised cardiovascular prevention...” Longevity expert Peter Attia tweeted recently. Do you agree with him? Is it a game changer?
The reality is more nuanced. CAC scoring has truly changed how we think about heart disease risk. Traditionally, we relied on cholesterol numbers, family history, and risk calculators — but these only gave probabilities, not evidence of disease. CAC shows you whether atherosclerosis (plaque buildup inside arteries) has actually begun. When used in the right patients, it’s the single best test we have to determine who truly needs aggressive heart disease prevention. It changes treatment decisions in nearly half of people who get it. If the score is zero, you might safely defer medication for a few years; if it’s high, that’s your cue to act early. But it doesn’t work equally well for everyone, and a zero score doesn’t mean you’re immune from heart disease.
What does the term ‘power of zero’ used with reference to this test mean?
CAC = 0 represents the strongest negative predictor we have in cardiovascular medicine. In people without symptoms, annual heart attack rates with CAC = 0 average 0.027% — translating to 99.4% survival over 10 years. The CAC Consortium tracked thousands of individuals and found death rates of only 0.32 to 0.43 per 1,000 person-years when calcium was absent. These numbers explain why many cardiologists call it the “power of zero.” It’s as close as we get to reassurance in cardiology. But that protection comes with an expiration date — it’s not forever. Think of it as a warranty period, not a lifetime guarantee.
How long does this ‘warranty’ last?
It depends on your risk profile. If you have diabetes, that protective window shrinks to just 3-4 years compared to 5-7 years for non-diabetics. In smokers, the benefit almost disappears. Current smokers with CAC = 0 have twice the cardiovascular death rate of non-smokers with zero calcium — the same risk level as non-smokers who already have moderate calcium buildup. The ‘power of zero’ evaporates if you continue smoking.
You said earlier that the reality is more nuanced. Can you elaborate?
People often think of calcium scoring as a yes-or-no test. But calcium represents only one-fifth of total plaque burden. The rest (soft, non-calcified plaque) doesn’t show up on a calcium scan. Under 40, most plaque hasn’t calcified yet. In fact, 58% of young patients with serious blockages have a calcium score of zero. So, if you’re 35 with chest pain or shortness of breath, a zero score doesn’t mean your arteries are clean. It means the disease isn’t calcified yet.
What about patients with genetic risks like high lipoprotein(a)?
That’s where things get interesting. Lp(a) predicts who will develop atherosclerosis in the future, while calcium scoring tells you who already has it. A recent study showed that people with high Lp(a) but CAC = 0 didn’t have higher near-term risk, meaning you can defer medication safely for now. But high Lp(a) means the process is still active underneath; you’ll need a repeat scan in 3-5 years to catch early progression. Calcium scoring gives you a snapshot in time; Lp(a) gives you the trend line for what’s coming next. Both matter, but tell different stories.
When does calcium scoring add value?
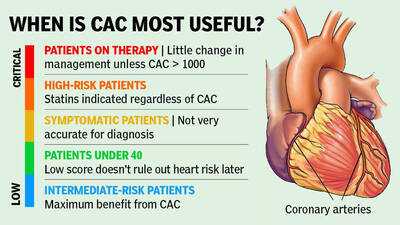
It offers the greatest clinical value for intermediate-risk adults between 40 and 75 — who fall in the grey zone where treatment decisions are genuinely uncertain. In studies, about half of them have zero calcium. For them, it’s reasonable to delay medications and focus on lifestyle. The other half discover visible calcium — and roughly one in four have scores above 100, which makes preventive therapy clearly beneficial. That’s the beauty of CAC: it transforms uncertainty into clarity.
And when does it mislead?
There are three key groups where calcium scoring can mislead. First, younger adults. As I said before, early disease often isn’t calcified, so the test can give false reassurance. Second, people with symptoms. If you have chest pain or shortness of breath, you need imaging that shows blockages directly, not just calcium. About 7% of symptomatic patients with CAC = 0 still have major soft plaque on detailed imaging — and among South Asians, that can go up to 28%. Third, very high-risk patients. If your 10-year risk is already above 20%, calcium scoring won’t change what we do.
How often should one repeat scan?
For most, five years is a good interval. If you have diabetes or smoke, three years. That’s because zero calcium today doesn’t prevent calcium accumulation tomorrow. In long-term studies, half of all people with a zero score developed calcium within ten years, and one in ten progressed to scores above 100 — enough to change their treatment plan.
There’s a lot of talk online about universal screening. What is your view?
That’s one of the biggest misconceptions. CAC works best as precision medicine — for people where we’re genuinely uncertain about prevention. It’s not for universal screening. If you’re already high risk, the result doesn’t change management. If you’re very low risk, it adds unnecessary radiation exposure.
If I got a zero-calcium score tomorrow, how should I interpret it?
Treat it as a green light to maintain what you’re already doing, not to stop caring. It’s reassurance, not immunity. Keep your cholesterol and blood pressure in check, avoid smoking, stay active, and get rescanned at the right interval. Zero calcium today tells you your arteries are quiet — but silence doesn’t mean safety forever.
“CAC has revolutionised cardiovascular prevention...” Longevity expert Peter Attia tweeted recently. Do you agree with him? Is it a game changer?
The reality is more nuanced. CAC scoring has truly changed how we think about heart disease risk. Traditionally, we relied on cholesterol numbers, family history, and risk calculators — but these only gave probabilities, not evidence of disease. CAC shows you whether atherosclerosis (plaque buildup inside arteries) has actually begun. When used in the right patients, it’s the single best test we have to determine who truly needs aggressive heart disease prevention. It changes treatment decisions in nearly half of people who get it. If the score is zero, you might safely defer medication for a few years; if it’s high, that’s your cue to act early. But it doesn’t work equally well for everyone, and a zero score doesn’t mean you’re immune from heart disease.
What does the term ‘power of zero’ used with reference to this test mean?
CAC = 0 represents the strongest negative predictor we have in cardiovascular medicine. In people without symptoms, annual heart attack rates with CAC = 0 average 0.027% — translating to 99.4% survival over 10 years. The CAC Consortium tracked thousands of individuals and found death rates of only 0.32 to 0.43 per 1,000 person-years when calcium was absent. These numbers explain why many cardiologists call it the “power of zero.” It’s as close as we get to reassurance in cardiology. But that protection comes with an expiration date — it’s not forever. Think of it as a warranty period, not a lifetime guarantee.
How long does this ‘warranty’ last?
It depends on your risk profile. If you have diabetes, that protective window shrinks to just 3-4 years compared to 5-7 years for non-diabetics. In smokers, the benefit almost disappears. Current smokers with CAC = 0 have twice the cardiovascular death rate of non-smokers with zero calcium — the same risk level as non-smokers who already have moderate calcium buildup. The ‘power of zero’ evaporates if you continue smoking.
You said earlier that the reality is more nuanced. Can you elaborate?
People often think of calcium scoring as a yes-or-no test. But calcium represents only one-fifth of total plaque burden. The rest (soft, non-calcified plaque) doesn’t show up on a calcium scan. Under 40, most plaque hasn’t calcified yet. In fact, 58% of young patients with serious blockages have a calcium score of zero. So, if you’re 35 with chest pain or shortness of breath, a zero score doesn’t mean your arteries are clean. It means the disease isn’t calcified yet.
What about patients with genetic risks like high lipoprotein(a)?
That’s where things get interesting. Lp(a) predicts who will develop atherosclerosis in the future, while calcium scoring tells you who already has it. A recent study showed that people with high Lp(a) but CAC = 0 didn’t have higher near-term risk, meaning you can defer medication safely for now. But high Lp(a) means the process is still active underneath; you’ll need a repeat scan in 3-5 years to catch early progression. Calcium scoring gives you a snapshot in time; Lp(a) gives you the trend line for what’s coming next. Both matter, but tell different stories.
When does calcium scoring add value?
It offers the greatest clinical value for intermediate-risk adults between 40 and 75 — who fall in the grey zone where treatment decisions are genuinely uncertain. In studies, about half of them have zero calcium. For them, it’s reasonable to delay medications and focus on lifestyle. The other half discover visible calcium — and roughly one in four have scores above 100, which makes preventive therapy clearly beneficial. That’s the beauty of CAC: it transforms uncertainty into clarity.
And when does it mislead?
There are three key groups where calcium scoring can mislead. First, younger adults. As I said before, early disease often isn’t calcified, so the test can give false reassurance. Second, people with symptoms. If you have chest pain or shortness of breath, you need imaging that shows blockages directly, not just calcium. About 7% of symptomatic patients with CAC = 0 still have major soft plaque on detailed imaging — and among South Asians, that can go up to 28%. Third, very high-risk patients. If your 10-year risk is already above 20%, calcium scoring won’t change what we do.
How often should one repeat scan?
For most, five years is a good interval. If you have diabetes or smoke, three years. That’s because zero calcium today doesn’t prevent calcium accumulation tomorrow. In long-term studies, half of all people with a zero score developed calcium within ten years, and one in ten progressed to scores above 100 — enough to change their treatment plan.
There’s a lot of talk online about universal screening. What is your view?
That’s one of the biggest misconceptions. CAC works best as precision medicine — for people where we’re genuinely uncertain about prevention. It’s not for universal screening. If you’re already high risk, the result doesn’t change management. If you’re very low risk, it adds unnecessary radiation exposure.
If I got a zero-calcium score tomorrow, how should I interpret it?
Treat it as a green light to maintain what you’re already doing, not to stop caring. It’s reassurance, not immunity. Keep your cholesterol and blood pressure in check, avoid smoking, stay active, and get rescanned at the right interval. Zero calcium today tells you your arteries are quiet — but silence doesn’t mean safety forever.
You may also like

Digital arrest: Couple forced to stay on video call for 3 days, duped of Rs 50.5 lakh; two held

Govt, PHDCCI hold pre-budget consultations focused on ease of doing business and MSME support

Cyclone Montha: Andhra CM Naidu visits affected areas in Konaseema district

Rajasthan HC grants six-month bail to rape convict Asaram on medical grounds

Sleeper bus accidents: IRF calls for strict adherence to code of bus body design






